Photo credit: U.S. Air Force Photo/Stacey Geiger
It is a good rule of thumb that if many treatments are in use for the same disease, it is because there is no real treatment known for that disease.- Peter Parish, Medicines: A Guide for Everybody
In the past, indeed until quite recently, people with IBS had appendix removals, intensive abdominal investigations, major gynecological operations, numerous x-rays, and prescriptions for a whole range of pills and potions to rid them of the strange collection of symptoms we now recognize as Irritable Bowel Syndrome. Not surprisingly, these drastic measures were not usually very successful since doctors were seldom treating the real cause of the problem. Luckily, things are different now.
The first thing your doctor will want to do is make sure that what you have really is IBS and not something else. Having done that, she will recommend treatment.
Even if you decide that you want to treat your condition yourself, or you want to receive treatment from a practitioner of alternative medicine, it really is most important that first of all you get a correct diagnosis from a qualified doctor. That way, you can be sure that you are treating the right thing and that nothing serious is being overlooked.
The first part of this chapter discusses the more typical examinations you may have. They may take place in your doctor's office or in a hospital outpatient department. It is unlikely you would have to stay in the hospital as an inpatient. If you are under about 40, the doctor may feel confident to make a diagnosis solely on the basis of your medical history and a brief physical examination alone, without arranging any tests. The second part of the chapter discusses the drugs and other treatments the doctor may recommend, having reached a diagnosis.
First, the doctor will ask you a series of questions. Your answers to the questions will often enable the doctor to decide whether you have IBS without the need to subject you to lots of tests.
You will probably be asked
*When did you first start getting these symptoms?
*Did anything specific trigger them?
*How often do they occur?
*Where exactly is the pain?
*Have you had diarrhea and/or constipation before?
*Do your bowel habits change?
*Have they recently changed?
*Have you lost weight recently?
*Does your stomach look or feel bloated or distended?
*Do you pass mucus with a bowel movement or even on its own?
*Have you ever had bleeding from the anus?
*Have you recently had a bout of gastroenteritis ('holiday tummy')?
*Did you get stomach aches as a child?
*Do any of your family have these symptoms?
*Do the symptoms become worse when you are tense, anxious, or under stress? Or when you eat particular foods?
*Can you do anything to make the symptoms better or worse?
*Do you or your family have an intolerance to dairy products or to wheat products? How much of these do you eat?
Depending on the answers and on your age, your doctor may suggest some physical tests. She may do some of them herself or refer you to a specialist. If you are under 40, she may want to check for a peptic ulcer, for gall bladder disease, ulcerative colitis, and Crohn's disease. If you are over 40, she will also want to be sure there is no sign of malignancy (cancer) in the bowel.
Because of the nature of IBS, it is not at present possible to do a single test that definitively confirms Irritable Bowel Syndrome. So, in some cases the doctor will want to do one or two investigations to rule out the diseases that IBS mimics before a firm conclusion can be made.
The first test will almost certainly be a rectal examination. The doctor will probably ask you to take off your clothes below the waist, lie on the examination table on your left side, and bend your legs up slightly. After putting on thin rubber gloves, the doctor will insert one finger into the rectum and feel around inside. This simple test will be able to tell the condition of your rectum. It will probably be a bit uncomfortable, and you may feel embarrassed, but don't forget that the doctor does this kind of thing every day. Good doctors will recognize your embarrassment and will do all they can to put you at ease.
Other likely investigations for IBS are blood tests, a sigmoidoscopy, and a barium enema.
Most people have had blood tests from time to time. A small area of skin, usually in the arm, is cleaned with an alcohol swab. A fine needle is inserted into a vein, and a small quantity of blood is drawn out into a syringe. The blood sample will be checked for generalized in fection, anemia, and the condition of the liver and kidneys.
A sigmoidoscopy is an examination to test for disease in the rectum and lower colon. You will need to have an almost empty digestive system for a sigmoidoscopy to be successful, so you will be asked not to eat anything for 24 hours beforehand. You will be asked to lie in the same position as for the rectal examination. The doctor will insert into the rectum one end of an instrument called a flexible sigmoidoscope, which is a very flexible tube one-half inch in diameter and about 24 inches long, with a light at the end. By shining the light into the rectum the doctor will be able to see clearly the condition of the rectum and the lower end of the colon. Any growths (cancerous or noncancerous) will be visible, as will any other abnormal condition such as inflammation. This examination, as you can imagine, can be quite uncomfortable and for some people may be rather painful. But most people who have it feel reassured that the whole area has been thoroughly examined. If, having looked, the doctor says that you do not have any inflammation or cancer of the rectum, you will probably feel greatly relieved.
A sigmoidoscopy has one other benefit: the process of inserting the tube into the rectum causes the rectum to become distended and often reproduces exactly the kind of pain you get with IBS. Many people are reassured to make the connection between a distended rectum and the pain of IBS and therefore are more motivated to take steps to avoid constipation.
A barium enema helps to check for organic disease of the whole colon and can also provide evidence of an irritable colon. You will need to have an almost empty digestive system for a barium enema to be successful, so you will be asked not to eat anything for several hours beforehand. You will be taken to the x-ray department, where a tube will be inserted into the rectum, and a small quantity of thick white liquid will pass through the tube. This procedure may be carried out on a table that allows you to be tilted slightly in different positions, so that the liquid can reach every part of the bowel. The tube is then withdrawn. The white liquid will show up brightly on the x-ray, and any problems or irregularities over the entire length of the large intestine will be clearly visible. If you have a spastic or irritable colon, this will also show up. After the x-ray, you will eliminate the white liquid as if it were a very runny and gassy bowel movement.
Some hospitals have a slightly different procedure: you will be asked to eat nothing after midnight and to take a laxative at bedtime. Next day you may have a simple x-ray of the abdominal area, and after that undergo the same procedure for filling up the intestine with the thick white liquid. Your intestines are then x-rayed. You may then be asked to empty your bowel for the whole area to be x-rayed again.
If diarrhea is your main symptom, you may also have tests for lactose intolerance and possibly a biopsy of the small intestine. For the bi opsy, you swallow a small metal capsule attached to a suction tube. When the capsule reaches the right part of the bowel, the doctor will apply suction to the tube, and a tiny piece from the wall of the bowel will be sucked into the capsule and removed for examination.
Just a word here about attitudes people have to tests in general. Most people are pleased to have tests to get reassurance that they have nothing seriously wrong with them; when the results are normal, they consider that the end of the matter. However, there is a small group of people who like having tests, who like having a hospital appointment to keep, who even like having operations. Are you one of these? If so, recognize it in yourself and realize that this behavior may cause you to receive less sympathy than you feel you deserve from your doctor, your family, and your friends.
In the past (and unfortunately even now occasionally), many doctors would say something like, 'We have done tests, and there is nothing wrong with you,' and leave it at that. If you still complained of stomach pain or changing bowel habits or a distended tummy, the doctor would probably dismiss you as a hypochondriac, prescribe tranquilizers, and hope you would go away. After all, tests prove that there is nothing wrong with you.
Today, particularly if your doctor is kind and caring, she may say, 'We will do some tests just to check that you haven't got disease A, B, or C, and I expect the tests will be normal.' So, when they are normal, this is just what you and she expect. And she will probably ex plain that you have Irritable Bowel Syndrome and will outline what it is, what it is not, how she can help you, and also how you can help yourself.
IBS cannot be helped by having an operation, but there are several types of drugs that are very effective. The most common are
'Antispasmodics to make the bowel muscle relax and to relieve the colicky spasm that causes so much pain. They appear to have no serious side effects, though they may impair driving ability or affect your blood pressure.
'Bulk-forming agents, usually based on the fiber psyllium. These make the stools soft, bulky, and easy to pass. They, too, appear to have no side effects.
* Antidepressants. Originally prescribed for the depression that af fects many IBS sufferers, some of these drugs also work di rectly to relieve abdominal pain and dampen the activity of neurons that send signals back and forth between the gut and the brain. Recent research confirms that these medications can be helpful even where depression isn't a problem. Since antidepressants must be used continually to be effective, they are generally only prescribed for the most drastic, chronic cases of IBS. Also, they often have side effects, and it is not in your best in terest to con tinue the long-term use of drugs that affect your mind.
* Experimental drugs, including a drug that blocks the brain's receptors for one form of seratonin. Seratonin is a neurotransmitter, a chemical substance that carries signals from all parts of the body to the brain. Among other things, this neurotransmitter is responsible for our perception of pain; the drug may help dull the perception of intestinal pain, which would benefit those IBS sufferers who are especially sensitive to pain in the gut. Another drug being tested by medical researchers is fedotozine, which numbs sensory nerves.
Where gas is a problem, peppermint oil capsules are often effective. You can obtain much the same effect yourself by sipping a few drops of peppermint essence in a small glass of warm water, or by sucking sweets containing oil of peppermint.
For diarrhea, you may be prescribed substances such as Lomotil, di phen oxylate, or loperamide.
For constipation, the most effective drugs are the bulk-forming agents, though you will probably be advised to eat more fiber in your diet. Don't be tempted to take laxatives that you buy over the counter. Un less used extremely rarely, they can make IBS worse.
For other ways to reduce stomach pain, see the next section.
The types of drugs mentioned previously are usually quite effective, particularly over a short period. But since IBS is often a long-term con dition, drugs alone cannot solve the problem permanently. If you can accept that what you eat, how you live, and how you view life will prob ably heal your bowel more effectively than anything else, you are already half-way along the road to recovery.
If you must take drugs, you should plan to do so for as short a time as possible. Once the bulk laxatives have given you a soft, un formed bowel movement every day for two weeks, see if you can make this happen by diet alone. For most people, this should be possible.
When you are confident that the antispasmodics have reduced your stomach pain, take a fresh look at the tension in you that is causing your bowel muscles to seize up. Then you will become less dependent on drugs. After all, if you see drugs as the only way of getting relief, you may feel a sense of helplessness and dependence on them. When you realize you can improve your condition for yourself, this will lift your spirits and help you take control of your own health.
You will find many ideas on how you can help yourself in this book. There is no suggestion, however, that you will find a permanent lifelong cure, because for many people this just will not happen. The longer you have had IBS, the harder it is to be rid of it completely. But there is no doubt at all that by handling it properly, you should be able to live more peacefully with it.
Once your IBS has been diagnosed and treatment (conventional or alternative) started, you will most likely not need to visit your doctor as often as you might have done before. But there are other causes of abdominal pain, and even IBS sufferers can get appendicitis, peptic ulcers, and heart trouble. Also, although IBS doesn't cause cancer, it doesn't prevent it either. So there are a few symptoms that, if they should occur, you must not ignore:
Blood in the stools or urine
Vomiting blood
Very severe abdominal pain
Indigestion-type pain that persists for more than a day or two
Excessive thirst
Unexplained loss of weight or appetite
Unexplained change in bowel habits that lasts for a month or more and causes disruption to your life
Unexplained increase in the size of your stomach
IBS symptoms that change or get noticeably worse
If you get any of these, see your doctor as soon as possible.
Do You Have Abdominal Pain?
Pain in the gut is what drives most people with an irritable bowel to the doctor. This pain is generally down on the lower left-hand side of the abdomen, but it could also be in the center or on the right. It may range from a dull ache to pain of such severity that the sufferer doubles up and even sometimes goes to a hospital emergency room. The pain may last from a few minutes to many hours and may be spasmodic or persistent. Once again, there are so many symptoms that it's not surprising it has taken so long for doctors to piece them all together into one recognizable condition.
The pain of IBS is generally colicky, cramplike, and spasmodic. The spasm may affect the whole bowel or just one section, so the position and intensity of the pain may vary. People with IBS will typically describe the pain as 'sharp,' 'stabbing,' 'knifelike,' 'burning,' 'cutting,' or 'very strong.' Some find the pain comes on after meals; those with diarrhea often find the pain comes on with the bowel movement and then gets better; those with constipation usually find that the pain only goes away when they stop being constipated. When the colon is distended (enlarged and stretched), this can produce pain in some unlikely parts of the body: the back, shoulders, thigh, and genitals. In contrast with this, some people with IBS find they get very little pain, just the other main symptoms.
Coping with Abdominal Pain
This section suggests ways of coping with abdominal pain. First, get it checked by the doctor. It is important to be sure your pain is due to IBS and not something else. Once you have your diagnosis, try these various ideas, and see which works best for you:
* Take antispasmodic drugs, as prescribed by the doctor.
* Take homeopathic nux vomica 6 or 30. Take two tablets one night, two the following morning, and two the following night, then stop. You should notice an improvement in two to four weeks; if your IBS recurs later, repeat this dose.
* When the pain strikes you, breathe deeply, concentrating on the passage of air in your nostrils and focusing your attention on a point between your eyebrows at the top of your nose. Exhale slowly. Try to keep your abdominal muscles relaxed the whole time -- do not tense them up.
* Lie flat, perhaps with your arms over your head if this feels comfortable, with a hot water bottle on your tummy. You may also find it helpful to use an electric blanket, though you should take great care when doing so.
* Lie on your back on the floor, head supported by a soft object, knees drawn up, and feet flat on the floor.
* Use a hot compress. Take a small towel, wring it out in hot water, fold it to a convenient size, and leave it on your ab domen until it cools.
* Do something active -- do some gentle stretching exercises or go for a walk. If you are in bed or in a chair, get up and walk around vigorously.
* Get rid of the constipation that might be the cause of the stomach pain.
* Do something to take your mind off the pain. If you have ever attended prenatal classes, practice the labor-pain exercises you learned. Otherwise, do something -- anything -- that requires concentration and makes you think of something else.
* Avoid antacid indigestion tablets. Their high-alkaline content destroys the stomach's natural acids, which digest food. If you take these tablets too often, the stomach responds by producing extra acid, which can cause more pain or digestive problems and eventually lead to a gastric ulcer.
* Infuse 1/3 to 2/3 ounce of hops (available from home-brewing shops and health food stores) in 1 quart of boiling water for ten minutes and drink a cupful after meals.
* Infuse 1/3 to 2/3 ounce of balm or lemon balm in the same way, and drink a cupful with meals.
* Heat a teaspoonful of fennel seeds in a cup of milk and drink it while fairly hot.
* When cooking, use herbs that aid digestion and that tonify and soothe the bowel. These include cumin, fennel, fenugreek, garlic, ginger, goldenseal, marjoram, mint, parsley, pau d'arco, rosehips, rosemary, sage, slippery elm, and thyme.
* Infuse 1/6 ounce of lavender in a quart of boiling water. Leave for five minutes, strain, and drink three cups a day between meals.
* Infuse four or five leaves of mint (dried or fresh) in a cup of boiling water, leave for five minutes, strain, and drink twice a day after meals. If this causes insomnia, use only two leaves per cup and drink one cupful a day, in the morning. You could also use peppermint essence oil in a glass of warm water.
* Infuse 2/3 to 1 ounce of fresh or dried thyme in a quart of water for about five minutes. Strain and drink three cupfuls a day after meals.
* Infuse 1/3 to 2/3 ounce of chamomile in the same way and drink three cups a day after meals.
* Try a preparation of skullcap or valerian root to calm the nerves that regulate the muscles of the intestine.
Most of these ingredients should be available from health food stores or large supermarkets.
The following homeopathic remedies may help cramping pains:
* Belladonna: if you feel distended but better when doubled up
* Bryonia: if you feel better when lying still and worse from heat
* Colocynth: if you can't keep still and feel better doubled up
* Magnesia phosphorica: if applying heat to your abdomen makes you feel better
If the pain is caused by gas, try the following ideas:
* Take steps to avoid constipation. A blocked rectum prevents gas from escaping, so it has no alternative but to build up in your intestines and cause discomfort. By keeping your rectum relatively empty, you allow that gas to escape.
* When gas builds up, sit up straight or stand up straight and, if possible, walk around vigorously.
* You may find a low-fiber diet helpful: more peeled vegetables; fish; lean meat; white rice, bread, and pasta; and less whole wheat bread or pasta, cereals, and dried fruit.
* Be aware that you may be swallowing excess air as you eat or drink -- try to avoid doing this.
* Infuse a cut root of angelica in boiling water for several minutes, strain, and drink a small glassful before meals.
* Chew raw angelica root or leaves.
* Chew mustard seeds with plenty of water.
* Put a few drops of peppermint oil in warm water and sip.
* Suck on sweets containing real oil of peppermint.
* Chew charcoal tablets.
* Add a teaspoon of cinnamon or nutmeg to warm milk, then sweeten with honey and drink.
* Infuse any of the following in boiling water for about ten minutes, and drink when it has cooled slightly (you may prefer the drink sweetened with honey): fresh or dried basil leaves, grated ginger root, half a fresh lemon, or some marjoram.
Exercises for General Improvement of the Abdomen
* This exercise strengthens all the abdominal muscles with a minimum of strain. Lie on your back with knees bent, feet flat on the floor. Clasp your hands behind your head, resting your head on your hands. Gently begin to sit up, without putting strain on your neck, raising yourself two to three inches until your shoulder blades are just off the floor. Hold this position for five seconds or longer. Breathe deeply. Repeat exercise several times. Listen to your body -- when your muscles ache, it's time to stop.
* Lie on your back with your knees bent and your feet flat on the floor close to your buttocks. Lift your hips off the floor, drawing the abdominal muscles up and in at the same time. Then lower your hips. Repeat several times; stop when you feel tired.
* Stand with legs apart, knees bent, hands pressing on thighs. As you breathe in, pull your abdominal muscles in and up, hold your breath, and pump your belly in and out using your muscles. Stop pumping when you need to breathe out, take a normal breath, then breathe in and repeat. Aim to do 10 to 15 pumpings at a time.
* Self-massage of the colon: lie on your back on a flat surface, and roll a tennis ball firmly up the right side of the abdomen, across the bottom of the rib cage, and down the left-hand side (that is, in the direction the digested food travels). This exercise is particularly effective if you do it first thing in the morning before rising.
* Cup one hand with fingers and thumbs closed tightly as if you were holding water in your hand. Then, keeping the hand in this position, gently strike your colon rhythmically with the hollowed hand and fingertips, keeping the wrists as loose as possible, with palm facing downwards. As in the pre vious exercise, work up the right side of the abdomen, across the middle, and down the left side. Do this exercise lying down.
Do You Have Constipation?
The symptoms of IBS are much more common in people with long-term constipation than in most other people. In fact, when people who do not have IBS are deliberately made constipated during research experiments, they start to develop some of the usual symptoms of an irritable bowel; and when their constipation is artificially ended by laxatives, their IBS symptoms cease.
Many people with IBS find constipation, either constant or intermittent, is their main symptom. In addition, they will probably have pain in the stomach, because the more constipated a person is, the more likely it is that he or she has abdominal pain.
One of the main causes of IBS is an irregularity in the speed with which food passes through the digestive system -- too slowly and you get constipation; too quickly and you get diarrhea.
What is constipation? Most people who get constipation would probably say that the stools are difficult to push out, that even after a bowel movement they have the feeling there is more to come, and that they don't have bowel movements as often as they think they should. Most doctors would agree that constipation is straining to pass the stools, having fewer than three bowel movements a week, and passing small, hard stools.
While most people have about one bowel movement a day, some have one every two or three days, some once a week. As a general rule, if your bowel movements are no more frequent than twice a day and no less frequent than twice a week, that is quite normal, provided that you have a soft, well-formed movement without pain or straining.
Generally, your bowel habits should remain fairly constant throughout your life, changing only when you have a change of environment, such as going on vacation or eating different food. If your bowel pattern remains unchanged, it is unlikely you have any disease of the digestive system. But if you have more constipation or more diarrhea that is not connected with a change in your lifestyle, and the change lasts for several weeks, it might be a good idea to see your doctor.
People with IBS often describe their bowel movement as 'like rabbit pellets,' or 'small, lumpy stool,' or 'stringy,' or 'hard and dry.' Let's look at why this happens.
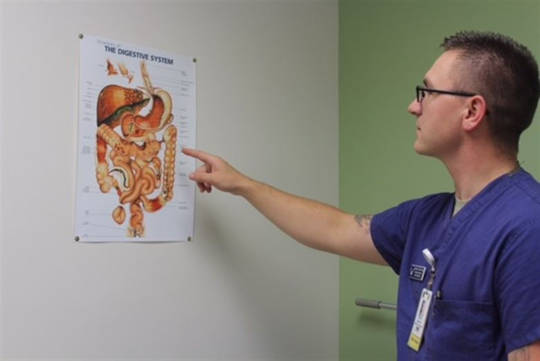
In the normal colon, feces are propelled along by peristalsis, in much the same way as food is propelled down the esophagus toward the stomach. (Remind yourself of your digestive system by looking at the diagram on page 20.) The muscle walls of the colon work best when they are propelling feces that are soft and bulky; this keeps the muscle walls a regular distance apart (remember, the colon is a tube). If the feces are small and hard, the colon must squeeze in further than its mus cular walls can comfortably manage. This causes pressure to build up and muscles to go into spasm in the colon, which causes pain.
When the muscle is in spasm, it no longer propels the feces in smooth waves toward the rectum. Instead, it just keeps squeezing and relaxing, often causing intense pain. And instead of the feces moving evenly on their way, they become compressed and divided into tiny seg ments with each squeeze, causing the typical hard, pelletlike stools of IBS.
Many people remain constipated for years. As a result, they are more likely to get diverticulosis, piles (hemorrhoids), and varicose veins. They may also have lower back pain or stomach ache from a rectum that is always too full with hard, compacted feces, not to mention extra problems such as headaches, lethargy, loss of appetite, and a general feeling of being 'under the weather.'
In addition, because food remains so much longer than normal in the digestive system, there is more chance for bacteria to build up allowing harmful materials to be absorbed into the bloodstream. With most people, food remains in the gut for about one-and-a-half to two-and-a-half days; for those who are constipated, food remains for an average of five days and may even last up to ten. Although unusual, some people with IBS can go a month without a bowel movement.
What causes constipation? As with most conditions, there are many causes. The most common are
*Lack of exercise
*Not enough dietary fiber in the diet
*Ignoring the call to empty the bowel
*Taking certain drugs
*Certain medical conditions
Many drugs cause constipation, so if you are taking any of the following and constipation is a problem to you, talk to your doctor about it:
*Pain killers (particularly the strong ones)
*Anticonvulsants (used in epilepsy and similar conditions)
*Water-reducing drugs (for heart conditions)
*Iron tablets
*Drugs for high blood pressure
Antacid tablets can also cause constipation, leading to a vicious cir cle: you have a pain in your stomach, so you take antacid tablets, so you may become more constipated, so you get more stomach pain.
Lastly, one of the main causes of constipation is, ironically, overuse of laxatives.
If Constipation Is Your Problem
If constipation is your problem, here is what you can do about it. The rules are quite simple, and for most people they will do the trick.
*The most natural treatment for simple constipation is a high- fiber diet.
*Drink plenty of fluids, preferably nonalcoholic and sometimes warmed. Tannin in black teas tends to constipate, so drink herb tea instead. There are some delicious ones available; if you find them a bit sharp, try adding honey.
*Drink at least 64 ounces of water a day.
*Some foods may make your IBS worse. If you suspect this may be so, try the simple diet on page 167 in order to identify which foods these may be.
*When you eat, a 'food-now-entering-stomach' message is sent to the brain. Then the brain sends a message to the intestines saying 'make room for an incoming meal.' This message causes the large intestine to empty its contents into the storage de pot of the rectum. So try to empty the bowel just after meals, when your body is preparing to move each batch of food along to the next stage. This system works most effectively after the first meal of the day, so be particularly aware of it after breakfast.
*Try to have your bowel movements at the same time each day.
*Allow plenty of time for each bowel movement. Try getting up twenty minutes earlier in the morning, eat a leisurely break fast, then disappear to the toilet with a book, magazine, or newspaper for at least 10 to 15 minutes. Don't push or strain, as this could cause piles (hemorrhoids); just allow time for the rectum to empty out.
*An early morning train, bus, or car journey may inhibit the natural morning urge to empty the bowels. So either fit in time for a long visit to the toilet before your morning journey or allow time for it when you arrive. A hot drink either before or during the journey may help to get your insides moving.
*Never neglect the urge to 'go.' When the rectum is comfortably full, the stools are covered with slimy mucus to make them easier to pass. But if the stools remain too long in the rec tum, this mucus is absorbed back into the body, making the stools hard, dry, and painful to pass. So when your body says 'go,' go! That way you work with your body, not against it.
*Since exercise is one of the things that triggers the bowel to empty, get plenty of it. This gives your brain a chance to send 'exercise' messages to the bowel. It needn't be wildly energetic; a brisk walk every day is fine for most people. Exercise also improves your capacity to withstand stress and keeps your internal muscles in good condition. Many digestive ailments are caused because muscles in the abdomen are too slack, so they sag, and the contents of the abdomen are compressed downward. This produces congestion, sluggish bowel movements, and constipation.
Here are some traditional remedies for constipation:
*Infuse 1/10 to 1/5 ounce of basil leaves or flower tips in boiling water. Strain and drink. Basil also has antispasmodic properties.
*Eat a raw apple in its skin for breakfast every day.
*Psyllium seed, with a full glass of water, keeps the stool soft.
*Drink barley juice or wheatgrass.
*Simmer two pounds of carrots in four cups of water for about one to two hours. Blend in a blender. Take as a soup.
*Soak figs or prunes overnight in water. The figs can be eaten uncooked, but prunes should be cooked before eating. Drink the water they have been cooked in, too.
*Eat kiwi fruit (a traditional remedy from New Zealand) from time to time.
*Eat charcoal biscuits (obtainable from pharmacists or health food stores).
*Drink a + cup of aloe vera juice in the morning and evening.
*Take natural licorice, as sweets or in stick form.
*Massage your lower back with a blend of essential oils: 20 drops of marjoram plus five drops of rose in two fluid ounces of vegetable oil. Essential oils can be obtained from many health food stores.
Do You Have Diarrhea?
As you will know by now, diarrhea is one of the main symptoms of IBS. You may have it on its own, or alternating with constipation, or with or without mucus. The usual pattern is to have a period of constipation with the typical 'rabbit pellets,' then out it all comes as a rather explosive diarrhea.
In fact, this is not typical diarrhea. Typical or infective diarrhea -- also known as gastroenteritis -- is usually caused by an infection or by con tam inated food or water. As the body tries to get rid of whatever has con taminated it, the typical symptoms occur: upset stomach, vomiting, abdominal pain, and great quantities of very loose stools. You will prob ably feel dreadful, all limp and washed out, but when you have gotten rid of whatever made you sick, you will start to feel better again.
The diarrhea of IBS is rather different. The quantity of feces that you pass is much smaller than with infective diarrhea; in fact, over sev eral days it is much the same quantity as an average bowel movement, though more frequent and sloppy. And the looseness is not caused by any infection or contamination.
With the diarrheal form of IBS, you probably get it worse in the morning and feel more settled as the day progresses. The pain may get worse as you have a bowel movement and then disappear. Also, you may have to get up in the night with it. Some people have IBS and diarrhea without any pain at all. Once again, there are so many variations that it's not surprising it has taken so long to link all the symptoms together.
It is possible that part of your colon does not work as well as it should and passes food on to the rectum before all the water has been properly absorbed, making the stools fairly runny instead of fairly dry. Also, your own rectum may not like being even half-full and may send 'emptying' messages too early.
Also, bear in mind that quite a large number of those with the diarrheal form of IBS use laxatives regularly and surreptitiously, and this is probably one of the causes of the problem.
Researchers have discovered that 50 to 60 percent of individuals with the diarrheal form of IBS have an intolerance to one or more foods. You may be one of these if you experience one of the following conditions:
*You have diarrhea as your main symptom.
*You wake up at night needing to have a bowel movement.
*You started to get IBS after an attack of gastroenteritis or a long course of antibiotics.
*You feel very tired or weary.
*You get headaches.
Whether diet is or is not an important cause of your IBS, if you have the diarrheal form of the condition, you most likely have more anxiety than those with the constipation form. After all, you know from those butterflies in your tummy before an important event what the link is between diarrhea and anxiety. So take positive steps to reduce stress and anxiety as a means of helping your irritable bowel. A later chapter on managing stress contains lots of ideas.
Here are some other well-tried remedies for diarrhea:
*Strange as it may seem, the same high-fiber/low-fat diet that is recommended for constipation also works for diarrhea in many people. Bran may work for you, although it may make the stools sticky for a few weeks.
*Bulk fiber supplements (such as Metamucil, Citrucel, or Fi ber all) help bind loose stools together.
*Antidiarrheal drugs prescribed by the doctor can be of great benefit, particularly if you get so agitated about being far from the toilet that your whole life is seriously restricted.
*Several herbs help: chamomile, slippery elm bark, blackberry root bark, and pau d'arco are beneficial. Use them in tea form. Ginger tea aids with stomach cramps and pain.
*Mix two teaspoonfuls of cider vinegar in a glass of water and drink before each meal.
*Before any event that is worrying you, try this: add one tea spoon ful of honey to one fluid ounce of hot water and stir until the honey melts. Then add two or three drops of essential oil of geranium (obtainable from health food stores) and sip slowly.
*Mix two heaping teaspoonfuls of arrowroot (obtainable from health food stores and pharmacies) with a small quantity of cold water until smooth. Top up with about one pint of boiling water and drink when cool. You may prefer it flavored, with black currant juice for example.
Beware of Laxatives
Many people use larger and larger quantities of ever-stronger laxatives more and more often, to less and less effect. They are afraid to stop in case they get more constipated; yet one of the main reasons for constipation is overuse of laxatives.
Laxatives are among the most common medicines bought over the counter. In addition, millions of laxatives are prescribed by doctors. Possibly up to 46 percent of the general population use them reg ularly. This is not only expensive, it is unnecessary and potentially harmful. And you would be surprised how many people with IBS regularly take laxatives and prefer not to tell their doctor.
Laxatives are extensively misused in the mistaken belief that there is some wondrous relationship between good health and a daily emptying of the bowels -- 'regularity is next to godliness.' This just isn't so. It is quite normal to have a bowel movement two or three times a day or two or three times a week. Even going one or two days over what is normal for you is nothing to worry about. As long as your movement is soft, well formed, easy to pass, and the same as it has always been, that's how it should be -- you are quite normal.
There really is no known connection between a daily bowel movement and good health. Nor does a less regular bowel-movement pattern indicate poor health, unless the change in pattern is recent, persists for several weeks, or has a noticeable effect on your life.
When you read advertisements for laxatives (whose manufacturers are, after all, trying to sell as much of their product as possible), it is easy to get the impression that missing a bowel movement is something really serious. So you become worried and take a laxative. This empties the whole of the large intestine, and several days pass before a normal quantity of stool forms again. In the meantime, you don't have another bowel movement because there's nothing in the bowel to pass, so you think you are constipated, and you take laxatives again. Thus you never give your body a chance to work normally. If this pattern continues, eventually the bowel muscle becomes damaged and won't work at all, unless there is a laxative to force it into action.
Ideally, the rectum will empty almost completely every day or so, as will about one-third of the contents of the large intestine. To empty everything all at once is not what your body was designed to do.
If you do take laxatives regularly, don't rush to cut down on them. Reduce the dose gradually, perhaps from two doses a day to one dose a day for a few days, then one dose every other day for several days, then two doses a week, then one dose a week, until you can finally stop completely without traumatizing your system.
There are several kinds of laxatives on the market. Some add bulk to the feces to make the bowel muscle propel them more easily; others loosen and lubricate the feces; others stimulate and irritate the bowel. The main types are
*Bulk-forming laxatives, usually made from fiber such as psyl lium, polycarbophil, or methycellulose (brand names include Meta mucil, Fibercon, Fiberall, and Citrucel). These are the ones most commonly prescribed for IBS and are the safest for long-term use. They stimulate the bowel muscles naturally by making the stools moist, soft, bulky, and easier to pass. (They may also help prevent diverticulitis.) Take plenty of fluids with them, as fluid keeps the psyllium soft and prevents it from becoming sticky. (Although the term bulk laxative is one that is still used, it may be a misuse of the word laxative. Fiber sup plements do not irritate the bowel, the function of a true laxative in stimulating the bowel. The proper term for these psyllium-based products are bulk-forming agents.)
*Lubricant laxatives, such as liquid paraffin. If you take these regularly, your body may fail to absorb some essential vitamins; they can also cause trouble with the bowel wall, liver, and spleen. Liquid paraffin coats some of the food you eat, thus preventing it from being properly digested and ab sorbed. It also prevents useful bacteria from working, it does not mix with water and so does not soften the feces, and, if you use it regularly, it may leak out through the rectum.
*Stimulant laxatives, such as cascara, castor oil, and senna. They increase bowel movements by irritating the lining of the bowel and stimulating the bowel muscles to contract. How ever, from reading the section on constipation, you now know that it can be very painful if the walls of the bowel contract excessively onto hard, compacted stools. If you have Irritable Bowel Syn drome, it is likely that your colon (or bowel) al ready contracts at a higher than normal rate, so laxatives of this type will probably make your stomach pain worse. Sti mulant laxatives can also be dangerous if, for any reason, you have an obstructed bowel.
*Saline laxatives, often called 'health salts,' make the stools bulkier by causing them to retain water (unlike bulk-forming laxatives, which make stools bulkier by causing them to retain dietary fiber). To do this, saline laxatives may draw fluids from the body and cause it to become dehydrated. They may be harmful to people with kidney disease or who are on diu retics (water-reducing drugs commonly prescribed for heart conditions). If in doubt, ask your doctor whether health salts are a good idea for you.
Finally, don't take laxatives to relieve stomach pains, cramps, or colic. These pains may signal a more serious condition, such as acute appendicitis.
Article Source
Staying Healthy with the Seasons
by Dr. Elson Haas.

Click here for more info and/or to order this book. Also available in a Kindle edition.
About the Author
 Elson M. Haas, MD, is an integrative family medicine practitioner with more than 40 years of experience as a physician. He is founder and director of Preventive Medical Center of Marin, an integrative healthcare clinic in San Rafael, California. Dr. Haas is author of a dozen popular books on health and nutrition, including Staying Healthy with the Seasons, Staying Healthy with Nutrition, The Detox Diet, Ultimate Immunity and, most recently, Staying Healthy with NEW Medicine. Learn more about Dr. Haas and his work at www.ElsonHaasMD.com.
Elson M. Haas, MD, is an integrative family medicine practitioner with more than 40 years of experience as a physician. He is founder and director of Preventive Medical Center of Marin, an integrative healthcare clinic in San Rafael, California. Dr. Haas is author of a dozen popular books on health and nutrition, including Staying Healthy with the Seasons, Staying Healthy with Nutrition, The Detox Diet, Ultimate Immunity and, most recently, Staying Healthy with NEW Medicine. Learn more about Dr. Haas and his work at www.ElsonHaasMD.com.
Books by this Author
at InnerSelf Market and Amazon