 A employee holds pre-rolled joints at Buddha Barn Craft Cannabis in Vancouver, Oct. 2, 2018. THE CANADIAN PRESS/Jonathan Hayward
A employee holds pre-rolled joints at Buddha Barn Craft Cannabis in Vancouver, Oct. 2, 2018. THE CANADIAN PRESS/Jonathan Hayward
The legalization of cannabis for adult use in Canada is one of the biggest national public policy shifts that many of us will ever witness in our lifetimes.
This historic change in drug policy was proposed by the Canadian government as a way to promote public health, as the country grapples with some of the highest cannabis consumption rates of the developed world, including among adolescents.
Meanwhile, Canada is struggling to contain an entirely different substance-related problem: The opioid overdose epidemic.
Fuelled by the contamination of the illicit drug supply with fentanyl and its analogues, the opioid epidemic is Canada’s gravest public health crisis since the emergence of HIV in the 1980s. Experts agree on the need for creative responses based on scientific evidence.
Increasingly, scientists from the fields of public health, medicine and economics are aiming to figure out if cannabis legalization could be part of the solution.
The possibilities are multiple — from the use of cannabis to treat chronic pain to the potential of cannabis to reduce opioid cravings.
We published a new study last month showing that highly marginalized patients on “opioid agonist therapy,” with the drugs methadone or suboxone, were more likely remain on their treatment six months later if they were using cannabis on a daily basis.
Opioids, cannabis and pain
Almost one in five Canadians live with some form of chronic pain. In the 1990s, pharmaceutical companies began to develop slow-release formulations of opioids (e.g. OxyContin) and marketed them as safe and effective medications for the treatment of chronic non-cancer pain.
Opioids are now known to carry a high risk of dependence and overdose and yet more than 20 million opioid prescriptions are still filled each year in Canada.
Drug overdoses are now the leading cause of death among Americans under the age of 50, and prescription opioids are involved in nearly half of these deaths.
It is also becoming apparent that opioids might be less effective than initially thought in treating certain types of chronic non-cancer pain (for example, neuropathic pain).
Cannabis, derived from the Cannabis sativa plant, contains several compounds. These include tetrahydrocannabinol (THC, the primary psychoactive component of cannabis) and cannabidiol (CBD). Beyond the well-known psychoactive effects of cannabinoids, new research has shown that they also interact with systems in the body involved in the regulation of pain.
This discovery has led researchers to investigate the potential for cannabis to treat various pain conditions for which opioids are currently first- or second-line therapies.
Although high-quality clinical research involving cannabis has been stunted by its prohibited legal status and the quality of the experimental studies in question ranges from low to moderate, recent extensive reviews of experimental research on cannabinoids for chronic non-cancer pain generally agree that they offer modest relief of pain.
This begs the question: if cannabis becomes more available, do people switch from opioids to cannabis?
Ground-breaking findings
In a landmark 2014 study, a team of researchers analyzed data from across the United States over a 10-year period. They found that states with legalized medical cannabis saw 25 per cent fewer opioid-related deaths than states where medical cannabis remained illegal.
These findings broke ground for others in the field to find associations between U.S. medical cannabis laws and reduced state-level estimates of opioid prescriptions, misuse and dependence, as well as opioid-related hospitalizations and non-fatal overdoses.
Opioid overdose trends have also changed in the aftermath of recreational cannabis legalization in some U.S. states. For example, a recent study found that opioid-related deaths in Colorado were reduced (albeit modestly) relative to two comparison states in the short term following recreational cannabis legalization.
Although it’s tempting to conclude that increasing access to cannabis is an effective intervention against the opioid crisis, there are several reasons to be cautious when interpreting these study findings.
First, not all cannabis laws are created equal. For example, Colorado and Washington followed a commercialized approach to cannabis legalization with fewer restrictions around things like marketing and product sales compared to Canada’s public health framework.
These regulations are likely to impact the ways in which people access and use cannabis products, which could create different shifts in other substance use trends.
 Prescription pills containing oxycodone and acetaminophen are shown in Toronto, Dec. 23, 2017. THE CANADIAN PRESS/Graeme Roy
Prescription pills containing oxycodone and acetaminophen are shown in Toronto, Dec. 23, 2017. THE CANADIAN PRESS/Graeme Roy
Indeed, a study led by leading drug policy economists in the U.S. found that the passage of a medical cannabis law on its own was not associated with changes in opioid-related outcomes. Only after the authors accounted for access to cannabis through legal provisions for retail dispensaries did they find a 25 per cent reduction in opioid-related deaths.
This suggests that if there’s a causal link between the law change and opioid overdoses, access to cannabis through retail outlets could be a driving factor.
Second — and this is the subject of ongoing discussion among substance-use researchers — these population-level studies are limited by their inability to observe individual-level changes in cannabinoid and opioid use.
As a result, it’s impossible to conclude whether it was actually the change in law that created these shifts in opioid outcomes. To better understand this, we need to take a closer look at different sub-populations of opioid users.
Pain patients and illicit users
Findings from surveys with medical cannabis users across North America demonstrate a clear preference for cannabis over opioids. For example, roughly one-third of a sample of patients enrolled in Health Canada’s Marijuana for Medical Purposes Regulations (MMPR) program in B.C. report substituting cannabis for prescription opioids.
For chronic-pain patients using medical cannabis, this substitution effect appears even more prominent, with cannabis substitution occurring in roughly two-thirds of a sample of former prescription opioid patients in Michigan who started using medical cannabis.
In another recent study, 80 per cent of medical cannabis patients in California reported that taking cannabis alone was more effective for treating their medical condition than taking cannabis with opioids. More than 90 per cent agreed they would choose cannabis over opioids if it were readily available.
However, two recent high-impact studies challenge our understanding of this complex topic. A four-year study of Australians on opioid therapy for chronic pain did not find significant reductions in use of prescribed opioids or severity of pain among cannabis users.
A second study analyzed a large U.S. dataset and found that individuals who reported cannabis use at baseline were actually more likely than non-users to start using prescription opioids non-medically and have an opioid use disorder three years later.
This discrepancy in findings points to a need for research exploring why this substitution effect is seen in some patient populations but not others.
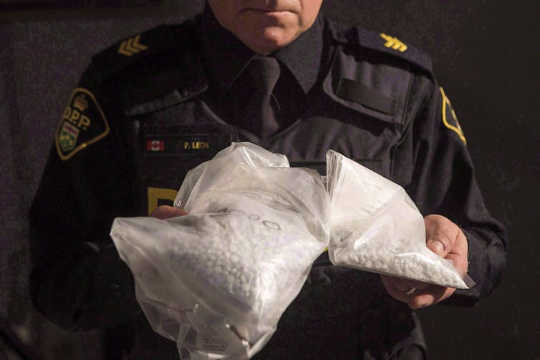 An officer displays bags containing fentanyl as Ontario Provincial Police host a news conference in Vaughan, Ont., in February 2017. THE CANADIAN PRESS/Chris Young
An officer displays bags containing fentanyl as Ontario Provincial Police host a news conference in Vaughan, Ont., in February 2017. THE CANADIAN PRESS/Chris Young
But what about the relationship between cannabis and opioids among some of those most affected by the opioid crisis — people with long-term experience using illicit opioids?
Untreated pain and substance use have a high degree of overlap. Pain was reported by almost half of people who inject drugs surveyed in a recent San Francisco study.
Research from our colleagues in Vancouver found that under-treatment of pain in this population is common and results in self-management of pain using heroin or diverted prescription opioids. This is becoming increasingly more dangerous, as almost 90 per cent of the heroin found in Vancouver is contaminated with fentanyl or fentanyl analogues.
Could there be a role for cannabis as an opioid substitute even among individuals with extensive experience using illicit opioids? A study from California of people who inject drugs found that those who used cannabis used opioids less often. We need more research, to know whether this is a direct result of cannabis use.
Cannabis as an addiction treatment
There is growing evidence for the use of cannabis in treating opioid addiction. CBD, the non-psychoactive component of cannabis, is known to interact with several receptors involved in regulating fear and anxiety-related behaviours. It shows potential for the treatment of several anxiety disorders.
Research is also investigating CBD’s role in modulating cravings and relapses — behaviours that are tightly linked to anxiety — among individuals with opioid addiction. Recent preliminary studies suggest that CBD reduces opioid cravings. A larger clinical trial is now under way in the United States.
Our own research suggests that patients are more likely to stay in opioid agonist therapy during periods of intensive cannabis use.
These findings suggest we need rigorous experimental research into the use of cannabinoids as an adjunct treatment to opioid agonist therapy.
Meanwhile, the opioid overdose crisis is so dire in some regions that community harm reduction groups, like the High Hopes Foundation in Vancouver’s Downtown Eastside, are starting cannabis-based substitution programs that provide free access to cannabis products for drug users.
Harnessing a unique opportunity
Canada is the first country in the G-20 to introduce a legal framework regulating the use of cannabis by adults.
Legalizing cannabis will break down historic barriers to understanding its clinical and public health impacts.
Certain measures like rates of youth use and impaired driving will no doubt be top priorities for evaluating the new law’s impact on population health and safety. But we should also be prepared to monitor indirect public health gains, especially against the backdrop of the ongoing overdose crisis.
Canada should harness this opportunity to understand if, and how, cannabis legalization could fit into a multi-faceted opioid prevention and response strategy.![]()
About The Author
Stephanie Lake, PhD student in Population and Public Health, University of British Columbia and M-J Milloy, Research Scientist, BC Centre on Substance Use and Assistant Professor in the Division of AIDS, UBC Department of Medicine, University of British Columbia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Related Books
at InnerSelf Market and Amazon



























